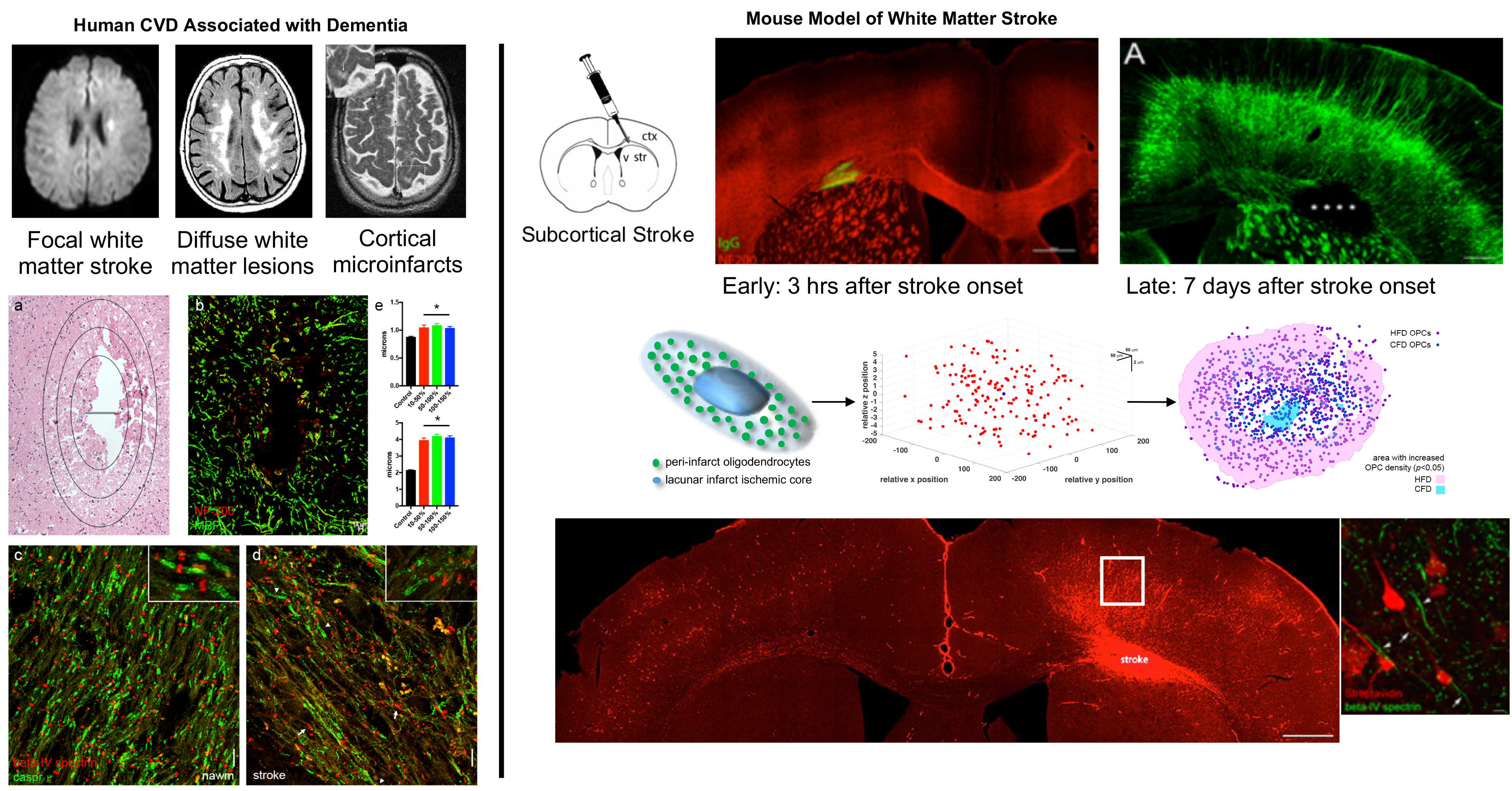
Cerebral microvascular disease is a pending public health crisis, accounting for 25% of the acute stroke patients presenting for care (~200K/year in the US) with an estimated 5-10 times as many patients suffering silent cerebral ischemia. Both obvious and silent strokes ultimately lead to age-related disability and dementia. There is increasing recognition that these cerebral microvascular lesions are provoked by chronic vascular risk factors including metabolic syndrome and show overlap with Alzheimer’s disease. Both of these areas are a focus in the laboratory. We have generated models of focal white matter ischemia and view a mouse model of metabolic syndrome as a diffuse white matter injury model.
Focal white matter stroke results in axonal degeneration that progresses over time. The laboratory is specifically interested in the role that oligodendrocytes play in this injury response. Ongoing work in the lab focuses on identifying oligodendrocyte molecules that stabilize and enhance axoglial interactions to prevent and repair this progressive degeneration. Collaborative work with the Carmichael Lab has identified a role for oligodendrocyte precursor cells in repairing focal white matter lesions by blockade of the Nogo signaling pathway.
Focal white matter stroke also uniquely injures the cortical neurons that have axons projecting through the stroke. Using retrograde labeling, we identified specific changes in the axon initial segment that occur in neurons injured after focal white matter stroke. Presently, we are using cell-specific isolation techniques to identify transcriptional changes driven by stroke in these neurons. This work will lead to the identification of specific molecular pathways that can both be targeted to prevent selective neuronal loss and injury as well as activate neuronal growth programs.